The IVF two-week wait (TWW) is often the hardest part of the entire fertility journey. After weeks of injections, blood tests, scans, egg retrieval and embryo transfer, everything suddenly goes quiet.
No more daily clinic visits. No more numbers. Just waiting.
This guide is designed to help you understand:
- What is actually happening inside your body after transfer
- Why symptoms are so confusing (progesterone vs. pregnancy)
- Evidence-based coping tools that can make these 14 days more bearable
- When you do need to call your clinic
It's not about "just relax." It's about having a plan for your mind, your body, and your days.
The Science: What Happens After Transfer?
Understanding the biology behind the TWW can reduce some of the fear and second-guessing. The following timeline describes a typical Day 5 blastocyst transfer (fresh or frozen) based on commonly accepted clinical guidance from bodies such as the American Society for Reproductive Medicine (ASRM) and the American College of Obstetricians and Gynecologists (ACOG).
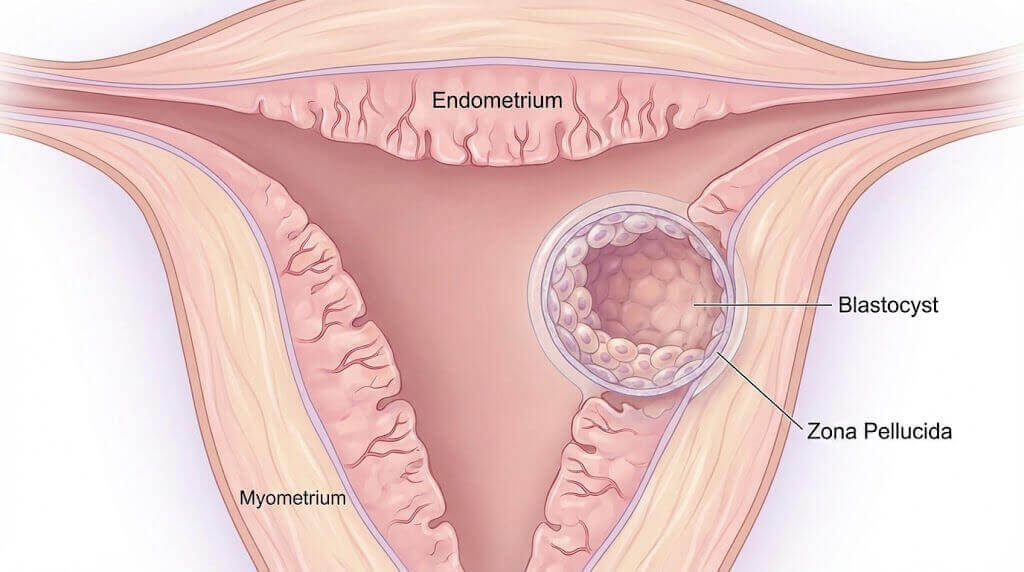
Days 1–3: Settlement and Hatching
- Day 1 after transfer:
The blastocyst continues to grow and starts to hatch out of its shell (zona pellucida). - Day 2 after transfer:
The embryo keeps hatching and begins to attach to the uterine lining (endometrium). - Day 3 after transfer:
Implantation begins. The blastocyst burrows deeper into the lining.
Some people may experience very light spotting, but many notice nothing at all.
Days 4–6: Implantation Complete
- Day 4:
Implantation continues; the embryo and endometrium are establishing a stronger connection. - Day 5:
Implantation is usually complete. Cells that will become the placenta and fetus have formed an initial blood supply. - Day 6:
Specialized cells start producing hCG (human chorionic gonadotropin), the hormone detected in pregnancy tests.
Days 7–9: Hormone Rise
- Days 7–9:
hCG levels begin to rise more steadily.
A very sensitive home test might show a faint line at this point, but false negatives are still very common.
Days 10–14: The Beta (Blood Test)
- By this phase, blood hCG tests (often called beta tests) can reliably confirm pregnancy.
- Clinics usually schedule the first beta 9–14 days after transfer, depending on their protocol.
The "Progesterone Prank": Symptoms vs. Side Effects
One of the cruelest parts of IVF is that progesterone, the hormone needed to support implantation and early pregnancy, causes almost the same symptoms as pregnancy itself.
That means your body can feel "very pregnant" even if the cycle doesn't work, and almost symptom‑free even when it does.
Common Symptoms in the TWW
| Symptom | Cause: Progesterone (medications) | Cause: Pregnancy (rising hCG) |
|---|---|---|
| Bloating | Very common | Common |
| Sore breasts | Very common | Common |
| Fatigue | Very common | Common |
| Cramping | Common (uterus adjusting, medication) | Common (implantation, uterine stretching) |
| Nausea | Sometimes (esp. high-dose progesterone) | Common (often starts around week 6+) |
| Spotting | Common (cervix irritation, suppositories) | Common (implantation or cervical changes) |
Key takeaway:
You cannot reliably tell if you are pregnant based on TWW symptoms alone.
- You can feel very pregnant and still get a negative test.
- You can feel nothing at all and go on to have a healthy pregnancy.
For more background on symptom timing and early pregnancy changes, see resources from Mayo Clinic and NHS "Pregnancy week by week".
A Realistic Day-by-Day TWW Mindset Plan
Medical timelines are helpful, but your mind needs a timeline too. Here is a suggested mindset focus for each phase of the TWW.
Days 1–3: "My job is gentle normal life"
- What's happening physically:
The embryo is hatching and starting to attach. You cannot "shake it loose" by walking around the house or going to the bathroom. - Mindset goal:
Shift from "I am fragile" to "My body knows what to do."
Practical actions:
- Move gently: short walks around the house or outside.
- Keep your routine light but normal: shower, simple meals, light work if you feel able.
- Save heavy housework, intense exercise, and lifting >10–15 kg for later, unless your doctor has cleared it.
Days 4–6: "Implantation is finishing; my job is stability"
- What's happening physically:
Implantation completes; the embryo is fully in the lining and beginning to signal hormonally. - Mindset goal:
Avoid obsessively checking for "twinges" or over‑analyzing every cramp.
Practical actions:
- If you journal, record facts vs. feelings:
- Fact: "Mild cramp lasted 2 minutes."
- Feeling: "I'm scared this means it failed."
- Limit Google time: set a 10–15 minute "search window" per day and stop when the timer ends.
Days 7–10: "Uncertainty peak; protect your mental space"
This is the emotional peak. Implantation is done, hormones are rising (or not), and your brain is screaming for answers.
- Mindset goal:
Accept that this is the no‑man's‑land of uncertainty—and build structures around yourself.
Practical actions:
- Decide in advance whether you will home test or wait for the clinic beta.
- Tell one trusted person (partner or friend) how you want them to support you:
- "Please don't tell me to just relax."
- "Please just listen; I don't need fixing."
Days 10–14: "Preparing for both outcomes"
- What's happening physically:
Blood tests can usually confirm pregnancy. Emotions may swing between hope and dread by the hour. - Mindset goal:
Prepare two scripts: one for a positive result, one for a negative.
Example scripts:
- If positive:
"This is the beginning of a new chapter. I can celebrate this moment even if I still feel scared." - If negative:
"This is a horrible outcome, and my feelings are valid. It does not mean I did anything wrong, and it does not erase my courage in getting this far."
Having the words ready in advance can make the phone call—or email—slightly less overwhelming.
Survival Toolkit: 5 Evidence-Based Coping Strategies
1. The "Warm Feet" Ritual
Traditional Chinese Medicine (TCM) often talks about keeping a "warm womb." While Western evidence is limited, many IVF patients find comfort in small rituals that help them feel cared for.
- Wear warm, soft socks or slippers.
- Use a light blanket while resting or reading.
- Keep drinks warm or room temperature instead of iced.
This isn't about magic; it's about grounding your nervous system with predictable, soothing sensations.
2. The 20-Minute Worry Window
Instead of fighting your anxiety all day, schedule it.
- Pick a specific 20-minute slot (e.g., 7:00–7:20 pm).
- During that time, you are allowed to worry, cry, Google symptoms, or write every fear down.
- When the timer ends, gently redirect yourself: stand up, drink water, change rooms, or call a friend.
This simple CBT-style technique, used in anxiety treatment, teaches your brain that thoughts can be contained, not erased.
3. Eat for Implantation (and Comfort)
You don't need a perfect IVF diet, but focusing on warm, anti-inflammatory foods can support both digestion and comfort.
Good options:
- Bone broth, warm soups, and stews
- Cooked leafy greens (spinach, kale, collards)
- Avocados, walnuts, almonds, olive oil
- Whole grains like oatmeal or brown rice
Limit (not ban):
- Iced drinks and large raw salads (harder to digest for some people)
- Highly processed snacks, ultra-sugary desserts, and energy drinks
- Excess caffeine and alcohol (follow your clinic's advice)
For general pregnancy nutrition principles, see Mayo Clinic – Healthy pregnancy diet.
4. Movement: Finding the "Goldilocks" Zone
Historically, patients were told to lie flat after transfer. Current guidelines from major fertility societies no longer recommend strict bed rest for most people.
Think not too little, not too much:
- Too little:
Staying in bed all day can increase anxiety, stiffness, and even reduce blood flow. - Too much:
High-impact workouts, running, or heavy lifting that your clinic explicitly told you to avoid. - Just right:
- Gentle walking 20–30 minutes a day
- Light stretching or restorative yoga (no deep twists or inversions unless okayed by your doctor)
- Normal daily life: cooking, desk work, light chores
Always follow your clinic's specific instructions, especially if you have risk factors like OHSS.
5. To Test or Not To Test at Home?
Home testing is one of the most emotionally charged decisions in the TWW.
Risks of testing too early:
- False negative:
hCG is still too low to detect, even if you are pregnant. - False positive:
An hCG "trigger shot" can stay in your system for up to 10–12 days, creating ghost lines.
Practical recommendations:
- If you must test, try to wait until at least day 7–8 post-transfer for a Day 5 embryo.
- Use an early-detection test from a reliable brand.
- Decide ahead of time how you will cope with any result and whether you will test again.
Ultimately, the blood test from your clinic is the only definitive answer.
Case Example: Emma's Second IVF Cycle
Names and details changed for privacy; based on common patient experiences.
Emma, 34, was on her second IVF cycle after a painful negative result the year before. During her first TWW, she:
- Googled symptoms for hours every day
- Tested at home from day 4 post-transfer
- Took every faint line and cramp as a sign—and crashed emotionally when the test was negative
For her second cycle, Emma and her partner made a different plan:
- She scheduled worry time for 15 minutes each evening.
- She wrote a short "script" for both possible outcomes with her therapist.
- She agreed to avoid home testing and wait for the clinic beta.
The TWW was still hard—but Emma reported feeling:
- Less out of control
- Less guilty about every symptom
- More prepared emotionally for the result (which, in her case, was positive)
Your story will be different. But like Emma, you deserve a plan that treats your mental health as carefully as your medications.
When to Call Your Doctor (and When to Breathe)
Mild cramping, twinges, and even occasional light spotting can be normal in the TWW—whether or not you are pregnant.
However, you should contact your clinic immediately if you experience:
- Heavy bleeding (soaking a pad in an hour, bright red bleeding)
- Severe abdominal or pelvic pain (not just mild cramps)
- Fever over 100.4°F / 38°C
- Sudden severe bloating, rapid weight gain, or difficulty breathing (possible signs of OHSS)
If you are unsure, it is always safer to call. Your care team would rather reassure you than have you suffer in silence.
For more background on early pregnancy safety, you can review:
- ACOG – Frequently Asked Questions on Early Pregnancy
- CDC – Assisted Reproductive Technology (ART) Safety
Planning Beyond the Wait
No matter how this TWW ends, you are not defined by this one cycle.
- If it's positive:
You may move quickly into blood test repeats, early scans, and a whole new set of worries. It is okay to feel both joy and fear. - If it's negative:
Grief is a normal, healthy response. Take time to process before rushing into next steps. Many patients find support in fertility counselors, patient groups, or trusted friends who "get it."
A Small Next Step You Can Take Today
If it feels safe to do so, you can gently look beyond the TWW:
- Use our IVF Due Date Calculator to understand how doctors calculate your due date from transfer date and embryo stage.
- Save useful resources (ACOG, ASRM, WHO, Mayo Clinic) in a bookmark folder labeled "Reliable Info Only", so you don't fall into random search rabbit holes.
You are not "overreacting." You are going through an objectively intense medical and emotional experience. Whatever the outcome of this TWW, the strength you are showing right now matters—and you deserve care, clarity, and compassion every step of the way.